Why I’m bringing AI to the bedside
Several years ago, I lost my nephew to sepsis — he was only 26 years old when this happened. It was devastating for my family. Sepsis is a life-threatening syndrome that is preventable only when it’s recognized early and treated in a timely way. Unfortunately, in my nephew’s case, it was recognized once his system was already in septic shock, a state where it’s much harder to rescue the patient.
I think about my nephew a lot. Because I know that everyone has a story like mine. With over 200,000 preventable deaths a year in the US, it’s incredibly likely that you, your neighbor or friend has lost someone dear to them at the hands of a preventable condition.
When my nephew was diagnosed with sepsis, my family called on me as I was the “sepsis expert.” Having spent over 5 years researching and creating AI / machine learning strategies to find early warning signs of life threatening conditions, focusing on sepsis, it made sense that I should have the answer. But I realized that my research was just that — it was research. It wasn’t impacting real world outcomes yet, but I knew it could transform the way care is delivered in the in-patient setting and save thousands of lives.
Right now, care is reactive, leading to conditions like sepsis being diagnosed too late. But it’s not the fault of our clinicians. Our clinicians are working their hardest but our system is not gearing them up for success. It’s not surprising that conditions like sepsis are missed. It’s hard to be by the patient’s bedside 24/7. Early signs can be subtle and providers rarely have time to click through dozens of screens culling data from this encounter and past encounters to determine patient specific baselines and hunt for subtle deviations that may be anomalous.
But, now is also a time when we can be building our systems for success. Interoperability rules are making it possible to stitch together a comprehensive longitudinal patient view. High quality artificial intelligence and machine learning driven systems can scan, analyze, and help focus attention to not miss critical events. The EMR provides a digital layer that spans nearly every care delivery setting and provides the infrastructure layer within which we can make care real-time, dynamic, patient and provider-context aware.
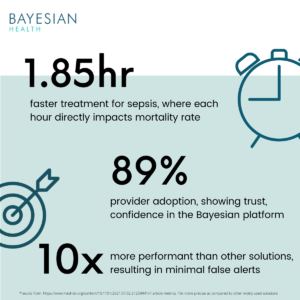
Done right, care can be better, more proactive, and safer while reducing provider burnout. This is exactly what Bayesian Health does. Just like the best providers continually integrate new data to refine their prognostication of what’s going on with a patient, Bayesian’s technology integrates every piece of available data to equip doctors and nurses with accurate, timely and trusted clinical signals that enable them to deliver the right care, at the right time, to save lives.
Bringing a Research and Science-Led Approach
Health AI is hard — the data are messy and challenging and requires approaches that draw signals that cut through the noise. Gaining provider trust and adoption is key to improving outcomes but they’ve been burnt on low quality solutions before. And how best to deliver these new kinds of solutions so it’s effective, safe, reliable, trustworthy requires new ideas, systematic measurement, and studies demonstrating use and efficacy. Bayesian’s platform is based on nearly two dozen studies (and counting) discussing novel algorithmic advances for improving precision, measuring and tackling bias, increasing quality of evaluations, and reporting. Further, we’ve run studies involving 4,000+ providers to date studying adoption and outcomes. This is the ethos with which we’re going to grow Bayesian — innovation, transparency, scientific mindset, and results.
I’ve spent my life’s work doing research in Artificial Intelligence, Machine Learning, and most recently with a focus in Human-Machine teaming. AI/ML are going through a renaissance — self-driving cars, preventing financial fraud, speeding up search, and enabling smart automation to improve our daily lives everywhere. In healthcare, we will see the same benefits.
Realizing improved patient outcomes isn’t easy. But I’m so optimistic for what’s possible when things are done right. Over the last five years, I’ve received hand written letters from patients and their families. These letters have fueled my desire to keep pushing, harder, to bring Bayesian’s technology to the bedside, helping patients just like my nephew.